We began fundraising for congenital heart defect (CHD) research the moment Graeme was born in 2012. That was when we first learned about congenital heart defects (CHDs). Nine years later, we started our own non-profit in his name, The Graeme McDaniel Foundation.
Our mission is to fund congenital heart defect research and support heart families.
The Graeme McDaniel Foundation is excited to grow and strengthen relationships with heart centers around the country. We are learning of these centers’ planned research projects and hearing how additional support from the foundation can progress their hard work. We will be able to choose which projects the foundation will support with the money you help us raise, and we are excited to share the progress and outcomes of these projects.
Please find the research grant application here.
Additional details can be found under the Medical Review Team & FAQs page.
Congenital Heart Defect Grant Awards
$94,272 to John P and Kathrine G McGovern Medical School at The University of Texas Health Science Center at Houston and Stanford University
The Role of Sex Chromosome Dosage in Heart Development: A Turner Syndrome Cardioid Model - Dr. Siddharth Prakash and Dr. Casey Gifford
The objective of this project is to understand the roles of sex chromosome dosage in heart development. Specifically, we propose to identify the molecular and cellular mechanisms that are perturbed when an embryo has less than two sex chromosomes and to understand how those changes are related to hypoplastic left heart syndrome (HLHS), bicuspid aortic valve (BAV), and other left-sided congenital heart lesions. We will create a new chimeric cardiac organoid differentiation model from Turner syndrome (45,X) induced pluripotent stem cells to identify cell lineages that are affected by reduced sex chromosome dosage. To determine the developmental windows and cell types where two sex chromosomes are required for cardiac development, we will mix 46,XX or 46X,Y and 45,X TS iPSCs at varying ratios and differentiate them towards cardioids. We will then quantify cardioid-level phenotypes as well as capture the single-cell transcriptome of mosaic cardioids to establish which specific cell types are affected by cardioid mosaicism. This will pinpoint the cell states that are disrupted by reduced sex chromosome dosage and establish minimum thresholds of mosaicism that cause these phenotypes. With this new organoid model, we are poised to deliver mechanistic insights that can explain sex differences in CHD risks and identify targets for potential new therapies.
2/3/2026 - It is known that one of the leading causes of miscarriage is improper formation of the heart in utero. There are many reasons for miscarriages, but the main cause is an incorrect number of chromosomes, or aneuploidy. The Prakash laboratory is interested in the effects of aneuploidy on heart development and how we can work to better understand why aneuploidy causes congenital heart disease.
To study aneuploidy, our lab makes stem cells from patients who are affected by Turner syndrome (TS), a type of aneuploidy condition with fewer X chromosomes than normal. Patients with TS have high rates of congenital heart disease. With guidance from Dr. Casey Gifford and her team at Stanford University, we turned cells from TS patients into cardioids, spheres of cells that can beat like an actual heart and are used to study why the heart may not develop properly. So far, we have learned that cardioids from patients with TS are smaller and beat less strongly than cardioids from other people. By studying these cardioids, we hope to discover why heart problems develop and find new treatments to correct or prevent heart disease.
$99,090 to Duke University
Investigating the Role of Cellular-Extracellular Dynamics in Partial Heart Transplantation - Dr. Douglas M. Overbey
Partial heart transplantation is a groundbreaking approach that allows transplanted heart valves to grow with pediatric patients. Duke is the leading center for partial heart transplant, with recent research focusing on expanding partial heart transplant therapy to the mitral position. This year we are investigating how the donor’s extracellular matrix and the recipient’s cellular response interact to influence graft viability and growth. These findings will help explain the science behind immune tolerance and graft ingrowth, which will assist with tailoring donor selection and improving long-term outcomes for children with congenital heart disease.
“Partial heart transplantation is transforming care for children with congenital heart disease. By understanding how donor and recipient tissues interact, we can move closer to personalized, long-lasting solutions for our patients.”
$100,000 TO CHILDREN’S hospital of philadelphia
Assessment of Cerebral Autoregulation Using Advanced Optical Neuromonitoring in Neonates with Congenital Heart Disease - Dr. Jennifer Lynch
The team at the Children’s Hospital of Philadelphia is pioneering new ways to protect the developing brains of newborns with critical congenital heart disease (CHD). With support from The Graeme McDaniel Foundation, they are advancing optical neuromonitoring tools that use near-infrared light to continuously track blood flow in the brain during surgery. These innovative tools allow clinicians to measure how well a newborn’s brain is maintaining stable blood flow despite changes in blood pressure, a key physiologic process called cerebral autoregulation. When autoregulation is impaired, the brain becomes more vulnerable to injury during surgery. By identifying these periods in real time, clinicians may be able to individualize cerebral perfusion strategies to reduce neurologic risk. The study will enroll 20 infants undergoing cardiac surgery for hypoplastic left heart syndrome. Using a noninvasive hybrid optical system, researchers will compute a new autoregulation index during critical phases of surgery and compare it to signs of injury on post-operative MRI. If successful, this approach could lead to safer surgeries, more informed clinical decisions, and better long-term outcomes for children with CHD.
“This generous award from The Graeme McDaniel Foundation will help us advance our goal of protecting the brains of our most vulnerable patients,” said Dr. Jennifer Lynch, Principal Investigator. “We’re excited to share this work with the broader pediatric heart community and build a future where fewer children suffer neurologic complications from life-saving surgery.”
1/25/2026 - Children born with complex congenital heart disease are at high risk for brain injury during heart surgery, yet clinicians currently lack real-time tools to assess how well the brain is being protected during these procedures. This project is studying a new, noninvasive monitoring approach that allows us to continuously measure cerebral blood flow during neonatal heart surgery.
Using advanced optical sensors placed gently on the infant’s head, we are able to track how the brain responds to changes in blood pressure and circulation. This response, known as cerebral autoregulation, is critical for protecting the brain during surgery. By identifying periods when this protective mechanism is impaired, we aim to better understand which infants are most vulnerable to neurologic injury.
Ultimately, this work lays the foundation for developing real-time monitoring tools that could help clinicians individualize care during surgery and improve long-term brain health for children with congenital heart disease.
During this reporting period, enrollment is underway, optical monitoring has been performed, data collection protocols are functioning as intended, and early datasets demonstrate the ability to compute cerebral autoregulation indices during cardiopulmonary bypass.
$57,000 to Johns Hopkins University
Fontan Plasma Metabolomic Phenotyping - Dr. Ari Cedars
As the number of individuals with the most complex forms of congenital heart disease, those with a Fontan circulation, continues to grow, healthcare providers are increasingly confronted with the reality that there are few if any proven treatments to prevent health deterioration in this unique population. The lack of treatment options is the result of an incomplete understanding of what exactly is happening in the bodies of Fontan patients that ultimately leads to health problems. If the scientific community can better define the things leading to deteriorating health in Fontan patients, then blood tests, drugs and devices might be developed to specifically target these factors which may improve their health outlook. With funding from The Graeme McDaniel Foundation, researchers at Johns Hopkins Hospital will investigate differences in the biological chemicals present in Fontan patients’ blood as a way to identify differences between those who are healthy and have a good exercise capacity and those who are prone to dying, being hospitalized or who have a poor exercise capacity. Because these biological chemicals reflect changes in many other bodily processes, these investigations will help identify new treatments directed at the various biological changes leading to deteriorating health in individuals with a Fontan circulation. By identifying those individuals who are at risk for experiencing health deterioration and pairing this with a mechanistic understanding of the cause of deterioration, we hope to begin to tailor therapy to the unique needs of each individual Fontan patient.
1/1/2026 - Using funding from the Graeme McDaniel Foundation, researchers at Johns Hopkins Hospital have been investigating differences in the biological chemicals present in Fontan patients’ blood as a way to identify differences between those who are healthy and have a good exercise capacity and those who are prone to poor health, being hospitalized or who have a poor exercise capacity. Thus far, we have identified different groups of Fontan patients based solely on their blood metabolite profile and are working to identify the implications of these differences for patients falling into each group. We have also identified certain blood metabolites specifically related to exercise capacity, the pumping function of the heart and the probabilities of hospitalization for heart problems or premature death. We are confirming these data, and are in the process of developing a novel approach to interpret the metabolite patterns associated with good and poor health (as opposed to looking at discrete individual metabolites) using machine learning to gain new insights. Through our work supported by the Graeme McDaniel Founation, we are making strides in identifying those individuals who are at risk for experiencing health deterioration and pairing this with a mechanistic understanding of the cause of deterioration. Using the data generated from this project, we hope to be able to tailor therapy to the unique needs of each individual Fontan patient.
“On behalf of the entire team at Johns Hopkins we wish those at The Graeme McDaniel Foundation a wonderful new year and thank you for your generous support for our project. We look forward to continuing to work with you to help improve the lives of congenital heart disease patients throughout the world!” Ari Cedars, MD
$95,420 to Boston Children’s Hospital
Simulation tool to predict outcome after biventricular repair - Drs. David Hoganson & Peter Hammer
Predictive Modeling for Safer Heart Surgery
Boston Children’s Hospital is grateful for the Graeme McDaniel Foundation’s partnership in our efforts to advance computational modeling to improve children undergoing complex biventricular heart repairs. Led by Dr. David Hoganson and Dr. Peter Hammer, the team is developing a patient-specific mathematical model that predicts how a child will respond to surgery—helping clinicians make more informed decisions about timing and surgical strategy. This model simulates a child’s circulatory system using real clinical data, enabling accurate forecasts of post-surgical heart function.
Ultimately, this work aims to make complex surgeries safer and more predictable, and to share the tool with hospitals across the country—ensuring more children receive the highest quality care, no matter where they are treated.
1/1/2026 - The team is looking to develop and validate lumped parameter models (LPMs) to predict if patients are ready for biventricular repair. In order to successfully employ the model, they need to understand how the left ventricle will respond to the loading changes from surgery. They can use a catheter procedure to get pressure-volume loop that will be used to show how the circulatory system performs under different conditions. There are 16 patients undergoing assessment for biventricular repair out of 100 that have PV loops. The team is in the process of validating the LPM model with these initial patients. Once the model can be customized for a patient with a match of the surgical outcome, this LPM can become part of the clinical process. This would give doctors a major tool that isn’t available today. They will be able to use the model to ensure that a patient is ready for surgery and also how well the patient’s repair will perform after surgery.
From the team, “We cannot thank you enough for your partnership in this groundbreaking journey to save young lives and revolutionize pediatric health care. Thanks to you, this team has made new discoveries and is preparing to launch new clinical modeling projects that we believe will have an enormous impact on the treatment of congenital heart disease long term. We can’t thank you enough for that support.”
$100,000 to UCSD School of Medicine/Rady Children’s Hospital of San Diego
Novel insights into the pathogenesis of hypoplastic left heart syndrome: Implications for treatment and prevention - Dr. Paul Grossfeld
Hypoplastic left heart syndrome (HLHS) is a heterogeneous group of disorders that is the most common cause of death in all infants born with congenital heart disease. The underlying genetic mechanisms are poorly understood. Dr. Paul Grossfeld and his team have identified several candidate genes for causing HLHS, using a combination of human genetics and animal model systems that are leading to novel insights into this disease. Their in vivo studies have demonstrated a highly conserved role for the cardiac endothelium in regulating cardiac myocyte proliferation and ventricular development in the pathogenesis of the most common form of HLHS. This information is transforming our approach into how we care for patients with HLHS, leading to improved care and the potential for prevention. Dr. Grossfeld and his team are honored to receive support from The Graeme McDaniel Foundation and would like to express their deepest appreciation for receiving this critical funding that will allow them to continue this very exciting research.
10/26/2025 - “Ets1-Regulated Endothelial-Secreted Factors Promote Compact Myocardial Growth and Contribute to the Pathogenesis of Ventricular Non-Compaction” has now been accepted for publication in the high impact journal Cardiovascular Research. This work was spearheaded by my project scientist in my lab, Dr. Lu Wang. It is the culmination of his most recent three years of work, following his previous publication in Circulation Research. In short, Lu has demonstrated that there are specific factors secreted by the cardiac endothelium (coronary vascular endothelium AND the endocardium) that are critical for normal ventricular development. Two of these cardiac growth factors have never been described before, and if we can get more funding, we plan to study further these factors not only for potentially treatment for defects in ventricular development, but also potentially for patients that have suffered a myocardial infarction, in order to promote cardiac myocyte regeneration. Thank you again for your wonderful support that has helped to make this possible! - Dr. Paul Grossfeld
$30,000 to Texas Children’s Hospital & University of Michigan Medical School
Single Nuclei Sequencing of PPVS Samples to Identify Differentially Regulated Genes and Pathways - Dr. Ravi Birla
Primary pulmonary vein stenosis (PPVS) is a serious congenital cardiac disorder where the pulmonary veins (PVs), which carry oxygen-rich blood from the lungs to the heart, become narrowed due to abnormal proliferation of vascular cells. The development of targeted therapies is greatly hindered as the molecular mechanisms driving recurrent stenosis remain unknown. As a result, the mortality rate of patients with PPVS is 40-50% within the first two years of life. In this study, led by Dr. Ravi Birla at Texas Children’s Hospital, we will elucidate the underlying pathophysiology of PPVS to develop an innovative therapy for this devastating disease and reduce the associated high rate of mortality. We will conduct single nuclei sequencing on PV samples from PPVS patients to identify differentially regulated genes and pathways. This will significantly increase our understanding of the underlying pathophysiology and lead to the development of potential therapies for the treatment of PPVS. Our long-term objective is to develop a targeted therapy for PPVS based on the pathophysiology of this disease and this study is an important step in this direction.
$50,000 to Texas Children’s Hospital, Baylor College of Medicine
Conversion of Congenital Single-Ventricle to Normal Two-Ventricle Circulation with A Magnetically Levitated Implantable Pump - Dr. Iki Adachi
Dr. Iki Adachi and Dr. Nobuyuki Kurita at Texas Children’s Hospital and Baylor College of Medicine are developing an innovative solution for children with single-ventricle heart defects. These patients undergo a series of surgeries to create unique physiology, the so-called “Fontan circulation”, which is named after the surgeon, Professor Fontan, who invented this life-saving surgery nearly 50 years ago. Although the Fontan operation has been considered as the ultimate goal of single-ventricle treatment, it is becoming clear that patients with the Fontan circulation are not free from long-term complications and, in some cases, premature death, due to the palliative nature of the unique circulation with single ventricle. To address the fundamental issue of Fontan circulation, ie. lack of a ventricle for the lungs, the team is developing the ReVolution Fontan Assist Device, a magnetically levitated sub-pulmonary pump designed to restore normal ‘two-ventricle’ circulation. This project involves the development of prototypes, in vitro testing, and design refinement, aiming to create a practical solution for this life-threatening issue. Support from The Graeme McDaniel Foundation is making this life-changing innovation to clinical reality.
$50,000 to texas children’s hospital
Development of the Lincoln Montano Stent for Fetal Cardiology - Dr. Michael Belfort
Dr. Michael Belfort at Texas Children’s Hospital has developed an innovative new stent, named the Lincoln Montano stent, for fetal intervention treatment on babies with hypoplastic left heart syndrome with restrictive or intact atrial septum (HLHS/RIAS). The current fetal intervention involves the placement of a stent designed for an adult coronary artery which can have disastrous repercussions if not placed perfectly the first time.
The Lincoln Montano stent can be placed percutaneously under ultrasound guidance through an 18 gauge needle. It is self-expanding and its specific barbell shape secures it in position once placed. During the placement, because of the detachable design which allows it to be removed and replaced as needed, the stent can be inserted and secured in the correct position much more easily than the current adult coronary artery stent. In the event it is not exactly where it should be it can be easily removed and redeployed without issue. Once it is correctly positioned it can be detached and left in place and the needle removed.
Support from The Graeme McDaniel Foundation will enable the team to make small modifications to finalize the prototype and proceed with preclinical testing in a live animal model (fetal sheep) and eventual bench testing for infectious and toxicology parameters, which will be the last remaining step before submitting the stent for approval from the FDA to use it in human fetal surgery.
“We are incredibly grateful to the Graeme McDaniel Foundation for their support of this project which will provide a new lifesaving option for intervention for babies with hypoplastic left heart syndrome before birth, revolutionizing the care these patients receive.” -- Dr. Michael Belfort
$91,170 to University of Arkansas for Medical Sciences, University of Colorado at Boulder
Optically Adjustable Pulmonary Artery Bands Made From Liquid Crystal Elastomer-Gold Nanorod Nanocomposites - Dr. Konrad Rajab and Tim White
This grant supports a multi-disciplinary effort to contribute adjustable pulmonary artery bands made from a newly developed “smart” material that changes shape when irradiated with light. The decisive benefit of this material over conventional approaches for adjustable pulmonary artery bands, such as electrical motors and hydraulic systems, is the simplicity of the resulting devices. This favors reliability and small form factors, both of which are essential for clinical application in pediatric cardiac surgery. Adjustable pulmonary artery bands will improve clinical care by perfectly balancing pulmonary artery blood flow at all times and thereby optimize cardiac and respiratory function of the affected children. If successful, this project will open new horizons for the treatment of children with congenital heart defects because the same “smart” material can also be used in other adjustable cardiovascular implants, such as shunts and fenestrations.
“Tim White is a thought-leader in the world of material science who invented a smart material that changes shape when exposed to light while he worked at the Air Force Research Laboratory. The tireless efforts of The Graeme McDaniel Foundation will allow us to leverage Tim’s incredibly innovative material to improve clinical care in the world of congenital heart defects.” Dr. Konrad Rajab, Congenital Cardiac Surgeon, Arkansas Children’s Hospital
$75,000 to Cleveland Clinic Children's and Georgia Tech
Uncovering Hidden Disease in Fontan Circulation: Noninvasive Detection of Diastolic and Pulmonary Vascular Dysfunction - Dr. Animesh Tandon, Dr. Petch Suntharos, and Dr. Omer Inan
The Graeme McDaniel Foundation funding will support work using wearable, noninvasive biosensors to uncover hidden forms of dysfunction in patients with single ventricle heart disease with Fontan circulation. We know from prior studies that patients with Fontan circulations have many forms of “hidden” problems, such as occult diastolic dysfunction and pulmonary vascular dysfunction, that contribute to worsened outcomes. So, we must find better, noninvasive ways of measuring subtle changes in heart function, over time, to catch when patients with Fontan circulation are developing hidden forms of dysfunction, including diastolic and pulmonary vascular problems.
We aim to correlate the noninvasive markers of cardiac function from novel, multimodal biosensors, to in-depth, relevant intracardiac metrics of diastolic and pulmonary vascular dysfunction in patients with a Fontan circulation through the use of pressure-volume loops.
When this work is complete, we expect to find markers of “hidden” cardiac dysfunction in patients with Fontan circulation that we can measure using wearable biosensors. This would then enable us to use these novel wearable biosensors over time, in the outpatient setting, to catch the onset of hidden dysfunction sooner than we currently can. This could then enable earlier interventions (surgery, catheterization, or transplant) to improve outcomes for this vulnerable population.
Wearable Sensors May Enable Everyday Monitoring of Congenital Heart Disease
$115,000 to polyvascular
Children born with congenital heart defects (CHD) often require pulmonary valve replacements early in life. Unfortunately, there are no transcatheter valve options on the market today that are sized appropriately for young children. Current solutions rely on open-heart surgery and the use of adult-sized or biologically derived valves, which are often too large, prone to early failure, and unable to grow with the child. This leads to a cycle of repeated surgeries throughout childhood. PolyVascular is working to change that by developing a polymer-based pulmonary valve specifically designed for young children, delivered through a minimally invasive catheter-based procedure. Their goal is to reduce the need for open-heart surgeries and provide a longer-lasting, more child-friendly solution.
Following the initial investment in 2023, PolyVascular completed a successful 90-day pre-clinical study that demonstrated excellent valve performance and durability. The results validated the promise of their pediatric transcatheter valve technology and positioned the team to prepare for their first-in-human clinical study. The Graeme McDaniel Foundation has now provided a second investment to help bridge this important transition.
This new funding will support three critical areas that must be completed before entering human trials: advanced computational modeling of the valve and stent to identify potential failure risks, manufacturing and sterilization of additional valves for regulatory-required testing, and biocompatibility studies to ensure the valve materials continue to meet safety standards. These milestones are essential for PolyVascular’s upcoming submission to the FDA and for setting the stage for clinical use.
“Funding like this is absolutely critical for the completion of pre-clinical work that will lead to first-in-human trials,” said Dr. Henri Justino, co-founder and Chief Executive Officer of PolyVascular. “We are incredibly grateful to The Graeme McDaniel Foundation for their continued partnership and shared commitment to improving outcomes for children with congenital heart defects.”
$100,000 to University of texas health science center and the children’s heart institute at children’s memorial hermann hospital
Tissue Engineering of Autologous Umbilical Cord Graft for Congenital Heart Defect Reconstruction - Dr. Damien LaPar
This proposal utilizes novel technology developed in the laboratory to address the limitations of currently available graft and patch materials. The team will utilize a portion of a newborn baby’s own umbilical cord that would normally be discarded as medical waste after delivery to manufacture novel graft material to utilize for future surgical reconstruction of that child’s own congenital heart or vascular defect. Use of the child’s own (autologous) umbilical cord graft (UCG) has unique and inherent advantages over autologous pericardium and/or foreign graft material. Additionally, using innovative and patented technology from the laboratory, they have developed techniques and protocols to quickly process and manufacture a newborn umbilical cord into a tissue patch that their lab has already utilized for repair of cleft palate and spinal cord defects. The team aims to extend the application of this technology to investigate its use in CHD reconstructions.
$50,000 to Texas children’s hospital heart center
Continued support of our 2023 Graeme McDaniel Research Scholar - Dr. Tam Doan
Thanks to ongoing support from The Graeme McDaniel Foundation, Graeme McDaniel Research Scholar Dr. Tam Doan at Texas Children’s Hospital will continue to expand his research on mitral annular disjunction, coronary artery anomalies, and fetal cardiology. Using new software called “TomTec AutoStrain” supported with funds from the Foundation, Dr. Doan and his colleagues are involved in several projects to study heart function in different disease processes. Dr. Doan will present research findings at the upcoming European Society of Cardiology Congress 2024 in London. He also continues to be involved with multi-center collaborations as well as collaborations within the Division of Cardiology and other departments at Texas Children’s with a goal to increase the quality of cardiology research.
You can read more about Mitral Annular Disjunction and Its Progression during Childhood in Marfan Syndrome in Dr. Doan’s paper here.
8/11/25 - Dr. Doan's research has produced three additional peer-reviewed publications and contributed to developing reproducible, clinically applicable imaging protocols. He has built new research collaborations across Texas Children's and beyond, with his work presented at leading national and international conferences, including the American Society of Echocardiography, Society for Cardiovascular Magnetic Resonance, American College of Cardiology, and Association for European Pediatric and Congenital Cardiology. Several of his mentees have also earned distinction through selected oral and poster presentations on LAS and CAA.
The LAS research has sparked exciting collaborations in 3D echocardiography and Al-enhanced imaging. Clinical uptake of MAD assessment has accelerated rapidly, with practitioners incorporating these findings into routine practice. Additionally, growing interest in Dr. Doan's work has led to mentorship invitations in Vietnam and Latin America, extending the reach of this work globally and helping build imaging capacity in regions where access is limited.
Graeme's story continues to inspire us all. The Foundation's investment in pediatric cardiology is a powerful tribute to his legacy and a beacon of hope for countless families. On behalf of Dr. Morris, Dr. Doan, and the entire Texas Children's Heart Center team, thank you again for your vision and partnership.
$100,000 to texas children’s hospital heart center
Using Fetal lung MRI and maternal hyperoxygenation to risk stratify in fetal hypoplastic left heart syndrome (HLHS) and total anomalous pulmonary venous return (TAPVC) - Dr. SHaine Morris
This project supports the work of Dr. Shaine Morris and the fetal cardiology team. Fetuses with hypoplastic left heart syndrome (HLHS) and total anomalous pulmonary venous connection (TAPVC) are at risk for developing obstruction to the normal drainage of blood from the lungs. This obstruction impairs normal lung development and markedly worsens the prognosis for the infants. While the overall structure of the fetal lungs can be assessed with routine fetal ultrasound, both fetal lung MRI and maternal hyperoxygenation testing offer valuable insight into the health of the developing fetal lungs. Both tests provide prognostic information on the postnatal course for infants and have been used in evaluation for candidacy of fetal interventions. However, little is known regarding how these tests change after successful fetal intervention, or how those changes impact fetal prognosis.
"We are so incredibly thankful for this gift that will truly allow us to push the field in fetal cardiology to help families affected by congenital heart disease to truly have the best possible outcomes!" Dr. Shaine Morris
8/11/25 - Dr. Morris and her colleagues have completed the most comprehensive analysis of fetal atrial septal interventions for HLHS worldwide, and the findings are now being reviewed for publication. The significance of this work has been recognized internationally, with presentations delivered in Frankfurt, Germany, and Prague, Czechia.
Additionally, Dr. Morris and her team are collecting data on fetal lung and brain development following cardiac intervention. Preliminary findings from this research have been accepted for presentation at the International Society for Ultrasound in Obstetrics and Gynecology (ISUOG) Scientific Sessions in Cancun, Mexico, in September 2025.
Dr. Morris also leads a multi-institutional collaboration under the Fetal Heart Society, focusing on lung health in fetuses with TAPVC. Data collection is well underway, with expectations for a high-impact publication. In parallel, her team has implemented a maternal hyperoxygenation testing protocol, a noninvasive procedure in which expectant mothers breathe high-concentration oxygen to assess how well oxygen is delivered to the fetus, helping predict postnatal outcomes. This testing has already been initiated in patients this year.
Technical Advances and Outcomes of Fetal Atrial Septal Intervention for Restrictive or Intact Atrial Septum Paper (The largest single center study to date on fetal atrial septal intervention in HLHS with severely restrictive or intact atrial septum.)
$50,000 to UH Rainbow Babies & Children's Hospital, Case Western Reserve University
Novel Zinc Bioresorbable Stent (ZeBRa Stent) for the treatment of vascular stenoses in pediatric patients with congenital heart disease - Dr. Martin Bocks
This project is proudly cofunded by a 3rd party event hosted in Ohio, Golf FORE CHDs.
Bioresorbable stents offer the potential for treatment of vascular stenoses without the concern for growth restriction as both re-stenting of the vessel with larger stents or vessel growth following vascular remodeling can occur once the stent material resorbs. This zinc alloy stent is very close to being the “holy grail” of stents for the treatment of vascular obstruction in patients with CHD. These stents should be strong, stay around to treat the obstruction for an ideal amount of time, and then resorb and disappear. This project will test a third generation of zinc coating. If successful, these stents could be used to treat any CHD that has associated vascular obstruction.
Golf FORE CHD Chair, Monica Nelson and Dr. Martin Bocks
$100,000 to Duke university
Partial Heart Transplantation: Expanding to the Atrioventricular Valves - Dr. Douglas Overbey
Partial heart transplantation represents a promising approach to provide growing heart valve replacements for newborn babies. The team’s previous groundbreaking work has shown partial heart transplants in the semilunar valve position grow with the recipient, providing the first ever clinical solution to the need for growing heart valves. They hypothesize that partial heart transplants can be performed in the atrioventricular (AV) valve position.
"Foundational research support in congenital heart surgery is incredibly important, since it allows us to pursue novel therapies for conditions that are relatively infrequent. These seed funds allow us to investigate new ideas that have enormous potential but not enough perceived impact or preliminary results to be competitive for larger scale funding avenues. Support from foundations tailored toward congenital heart disease is a great way to push forward innovative therapies that could help many future children with congenital heart disease. We are incredibly excited to be a part of these studies and look forward to honoring the foundation." Dr. Douglas Overbey
2024 Update - Dr. Overbey shared this PCICS podcast discussing partial heart transplant and that experiments from the most recent submission are going very well. They have finished the mockup models and are working on live animal experiments - more to come!
https://pcics.org/news-resources/podcast/
Episode 113: Partial Heart Transplantation
Guests Dr. Douglas Overbey, Dr. Katie Cashen, and Dr. Erin Shea from Duke University discuss partial heart transplantation of pediatric semilunar valves.
Co-hosts Deanna Todd Tzanetos, MD, MSCI and Misty, Ellis, DNP,APRN, CPNP-AC/PC (Norton Children's Hospital/U of Louisville)
Editor/Producer: Deanna Todd Tzanetos, MD, MSCI (Norton Children's Hospital/U of Louisville)
1/27/25 - Dr. Overbey on the TODAY show highlighting the incredible work happening at Duke
5/6/25 - “We were able to identify growth of the valve on serial echocardiography, and perfect the technique. This gave us the necessary confidence and knowledge to move the innovation into humans. In January 2025, a 14 year-old female received the world’s first mitral valve partial heart transplant. This would not have occurred without funding from the Graeme McDaniel Foundation.” - Drs. Overbey and Turek
$50,000 to University of texas health science center and the children’s heart institute at children’s memorial hermann hospital
Cellular Signaling and Stem Cell Therapy in Congenital Heart Disease - Dr. Damien LaPar
During the first year of support, Dr LaPar's team has successfully developed an in vitro model of endocardial fibroelastosis (EFE). EFE is the scarring in the developing heart that commonly occurs in patients with CHDs. This year, the team will continue their work in an attempt to eventually stop or reverse the formation of EFE through stem cell therapy.
$50,000 to Texas children’s hospital heart center
The Graeme McDaniel Research Scholar (year 2) - Dr. Tam Doan
The Graeme McDaniel Research Scholar will be awarded to one of Texas Children’s Hospital’s faculty over a period of one year to support their work in preparation for future applications for ongoing congenital heart defect research funding. Through this mechanism, the fund will achieve significant financial leverage through its support of bright early-career researchers enhancing their ability to obtain career-defining long-term research funding. The potential to follow these advanced individuals and maintain relations with them as they grow in their career is invaluable. With a 3-year commitment, we look forward to funding three Graeme McDaniel Research Scholars.
We are honored to announce Tam T. Doan, MD, MS, RDCS as our 2nd year Graeme McDaniel Research Scholar!
Dr. Doan’s primary clinical focus lies in fetal cardiology, diagnostic and interventional echocardiography, and cardiac MRI. Additionally, he is dedicated to caring for youth with coronary artery anomalies and has had a research interest in myocardial stress perfusion assessment. He actively engages in research initiatives, exploring new technologies in cardiac imaging and leveraging artificial intelligence and machine learning to analyze cardiovascular images and patient data.
"It has been a wonderful experience learning about the Graeme McDaniel Foundation, the McDaniel family's journey, and Graeme's legacy. I'm sincerely grateful to the foundation for affording me the opportunity to reflect on my personal path and passion in pediatric cardiology. Most importantly, your inspiration and provision of cutting-edge technology have equipped me to study heart function with novel approaches which could potentially enhance the diagnostic toolkit for early detection of clinical decompensation and improve patient outcome. We feel honored to present our work as a moderated poster at the Annual Scientific Sessions of the American Society of Echocardiography in Portland, OR (June 2024). We have submitted another abstract utilizing left atrial strain as a novel marker to predict outcomes in patients with unrepaired congenitally corrected transposition of the great arteries and anticipate feedback in May 2024.
I am sincerely motivated by the opportunities to make meaningful impacts on the lives of young patients and their families by implementing best clinical practices and advancing our understanding and treatment of pediatric cardiac conditions through clinical research and education." -Dr. Doan
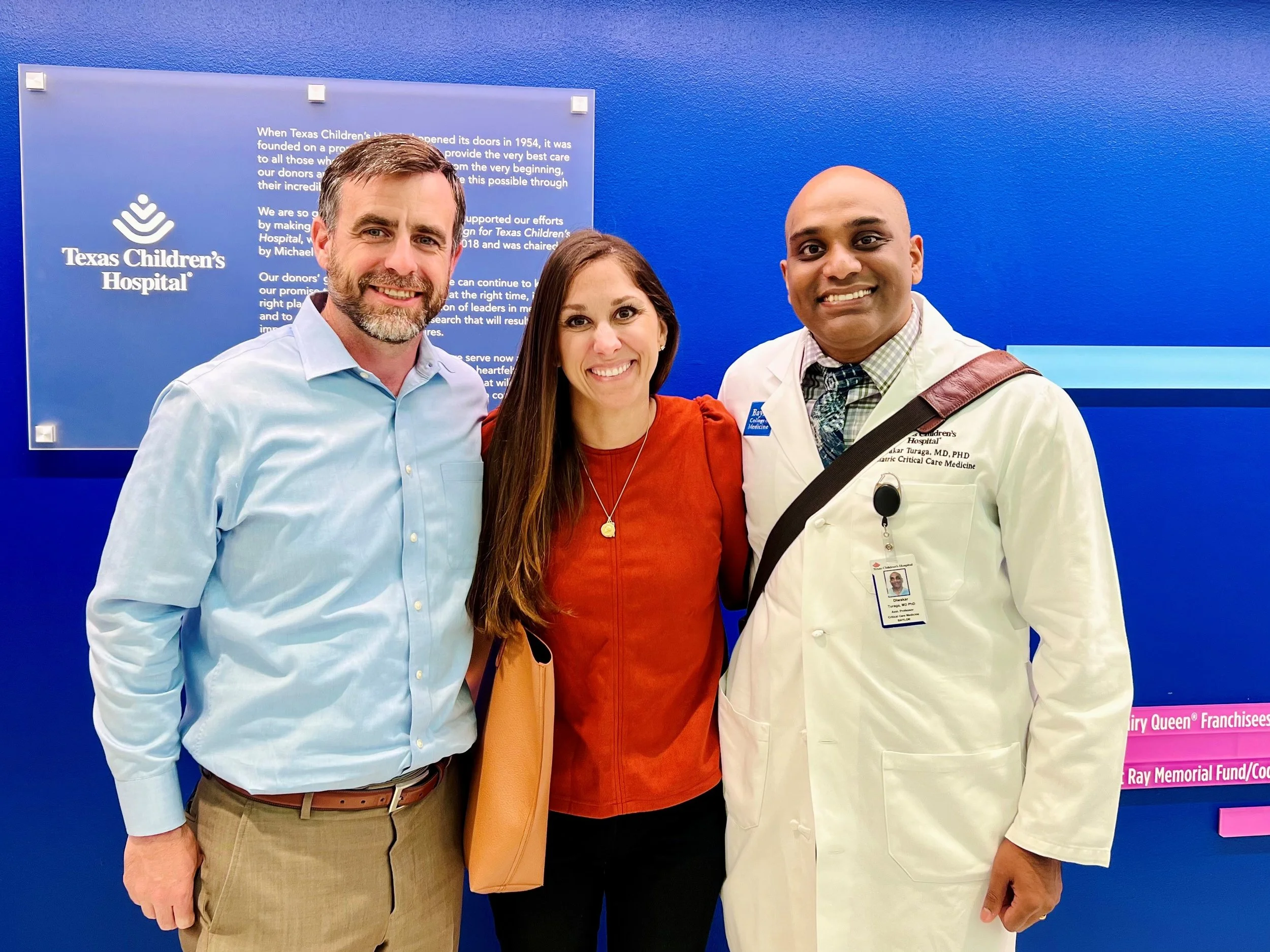
$50,000 to Texas children’s hospital heart center
continued support of our first Graeme McDaniel Research Scholar - Dr. Diwakar Turaga
Dr. Turaga was our 2022 Graeme McDaniel Research Scholar. After learning more about his findings and touring his lab, we were excited to continue supporting his groundbreaking research. "Complex congenital heart disease (CHD) patients invariably require complicated surgical repairs. Despite the best possible surgical repair, some of the patients develop heart failure. My research is focused on applying cutting edge genomic tools to understand why the heart muscle fails in these patients. The CHD heart muscle faces abnormally high amounts of stress and works tirelessly, and our recent results show that the CHD heart muscle ages faster than expected. Now that we have an insight into why these CHD hearts fail, we can start working on making the heart muscle stronger [by using precision medicine]." Dr. Turaga
In certain serious conditions like congenital heart disease, the RV may pump blood into the body instead of just to the lungs. In very rare cases, some people have what's called a 'super RV', where these stressed RVs continue to function well even into later stages of life. In this study, we looked at the genetic activity of ‘super RV’ from a 60-year-old person who had a specific type of congenital heart defect called congenitally corrected transposition of the great arteries (ccTGA). We found that in this person's RV, there were two important pathways that were more active than usual, a pathway related to insulin-like growth factor (IGF1) was more active and increased activity in pathways related to the growth of new blood vessels (angiogenesis). These findings suggest that in rare cases, the RV might last much longer by adapting to the extra strain by becoming more responsive to growth signals and by growing new blood vessels. Understanding how the RV adapts to increased stress is important for developing better treatments for congenital heart disease. Now that we know 'WHAT' genes to target, next steps will be 'HOW' to target the genes in the heart. We can potentially repurpose existing drugs which target these pathways (used for cancer, endocrine diseases) to treat RV failure or use gene therapies to specifically treat heart cells. Both approaches are promising, now that we know 'WHAT' to target. The detailed paper can be found here.
Congratulations, Dr. Turaga, on receiving the 2025 Catalyst to Independence Award!
$ 50,000 to boston children’s hospital
3D MODELING AND FLOW SIMULATION FOR COMPLEX CONGENITAL HEART DISEASE - Drs. David Hoganson and Peter Hammer
The team at Boston Children's Hospital has created a program that uses imaging to create computational fluid dynamics (CFD) models of patients’ hearts. With these models, the team can offer much greater care to children that require surgical interventions. The models enable surgeons to simulate surgical repairs. In addition to having a much better idea of the patient’s specific anatomy before conducting the surgery, the team can use these modeled repairs to see how flowrates and pressures in the heart will react to the planned surgery. Another important use for these models is to give a much more detailed measurement for cutting 2D patches that surgeons will install into a 3D heart. Without the model, the surgeon is often making corrections to the patch during the actual surgery. The model can also be used to simulate how any surgical repair will react as the child continues to grow. With the money from The Graeme McDaniel Foundation, the team at Boston Children's Hospital will be able to hire additional engineers to expand the program and service more children. The ultimate goal is to roll this process out to major heart hospitals all across the country. This video focuses on the collaboration between engineers and surgeons, and the tremendous impact their work has had on so many families.
2023 Update “Support from the Graeme McDaniel Foundation has been critically important as we extend our clinical 3D modeling program into computationally planning patches for repairs inside the heart and can take those plans into the operating room for the surgeon to use as a guide to determine the shape and size of the patch. This is a very exciting advancement to improve the geometric and clinical outcomes of some of our most complex repairs.” Dr. Hoganson
2024 Update Dr. Hoganson and his team were able to use the grant from The Graeme McDaniel Foundation to further their work using computational fluid modeling to treat CHDs. The team has been able to begin modeling complex mitral and tricuspid valves in CHD patients. The team was also able to hire an engineer to focus on using computational 3D modeling to design complex patches. Finally, they have also used the 3D modeling to show that many Fontan patients would benefit from upsizing the Fontan conduit as single-ventricle patients grow. By defining who would be a candidate for this procedure, many patients could have less long-term liver damage.
Final Update As we near the close of 2024, BCH will have modeled 1,500 pediatric hearts—300 more than we reported in June. In early 2025, the team will focus on a critical need for newborns with coarctation, a condition where a narrowing of the aortic arch impedes blood flow. Through the use of 3D modeling, surgeons will be able to precisely measure and create the necessary patch to repair the aortic arch, using cutting-edge laser guiding technology to ensure the patch is placed with pinpoint accuracy. In collaboration with industry partners, the team has developed a patch made from adult pulmonary arteries, allowing it to stretch as the child grows, effectively eliminating the need for future surgeries and significantly improving the long-term health and life expectancy of these children. While the progress at BCH has been incredibly promising, Dr. Hoganson and his team are committed to ensuring that this life-saving work extends far beyond our hospital. Their vision is to bring these benefits to institutions across the nation and around the world. Just this fall, they succeeded in getting billing codes approved for 3D modeling, virtual surgery planning, and flow simulations, a vital step toward ensuring that this work can be sustained long-term. For our patients with congenital heart disease, every millimeter matters. This groundbreaking technology is helping us achieve the best possible outcomes, ensuring that our young patients not only survive but thrive. Learn more here: BCH Blog Article and NY Times Podcast - Episode 4.
$100,000 to polyvascular
A large percentage of CHD patients require valve replacements. The good news is that valve repairs have improved greatly over the years. The bad news is that there isn’t a good source of artificial valves for doctors to use on young children. Typically, the goal is to give the child enough time to grow large enough that the smallest available adult valve can be used. The problem is that these valves are still typically too large, and they can cause issues that require additional intervention. PolyVascular is a company founded by doctors with the goal of developing artificial valves that are sized specifically for small children. Because the market for adult valves is so much larger than valves for young children, these children’s valves have never been able to attract enough funding to get a product from design all the way to market. By raising money from The Graeme McDaniel foundation and others, PolyVascular will develop a valve that is specifically designed for small children. They will pair the valve with a delivery system that will allow the valve to be placed by catheter instead of open-heart surgery. Hospital time will be greatly reduced and future complications from a poorly sized valve will be eliminated.
2023 Update In the six months since receiving funding from The Graeme McDaniel Foundation and other supporters, PolyVascular has made significant strides in advancing their mission to develop artificial pulmonary valves tailored for small children with congenital heart defects. The Graeme McDaniel investment has helped fuel extensive valve testing and the beginning of a robust pre-clinical study.
Valve testing includes ensuring the deliverability, performance, and durability of the valve design. Valve testing is a rigorous process starting with the careful manufacturing and inspection of the valve. These benchmark tests help PolyVascular to ensure the highest quality standards are met for their valves. Testing over this time showed favorable results, exciting the team as they moved into the pre-clinical study.
The 90-day pre-clinical study began at the end of 2023 and is ongoing. Initial results from the study yielded remarkable achievements in performance and durability.
The valve testing and pre-clinical study mark two very significant achievements for the team. These two milestones were met due to the amazing support of our investors including the Graeme McDaniel Foundation. PolyVascular is excited to continue their work in 2024 and report further success!
$100,000 to University of texas health science center and the children’s heart institute at children’s memorial hermann hospital
Cellular Signaling and Stem Cell Therapy in Congenital Heart Disease - Dr. Damien LaPar
The proposed research plan will provide critical data related to the underlying inflammatory signaling mechanisms and downstream cellular effects that promote the deleterious development of endocardial fibroelastosis (EFE) and scarring in the developing heart. A new in vitro model of EFE will serve as a novel experimental platform to support the development of future treatment and therapeutic options for affected babies. The primary goal is to investigate cellular mechanisms to identify progenitor cell (stem cell) - based therapies to combat scarring of the inner surface of the heart that leads to abnormal functioning and development of the heart in congenital heart disease.
As lead scientist, Dr. Damien J. LaPar MD, MSc states, “We believe that by understanding the underlying mechanisms, we are going to be able to develop cellular and regenerative therapies either through stem cells or pure cellular-level signaling cascades that could arrest that process, [then] reprogram those scar-forming cells so they can form [healthy heart] muscle.”
$50,000 to Texas children’s hospital heart center
The Graeme McDaniel Research Scholar (year 1) - Dr. Diwakar Turaga
The Graeme McDaniel Research Scholar will be awarded to one of Texas Children’s Hospital’s faculty over a period of one year to support their work in preparation for future applications for ongoing congenital heart defect research funding. Through this mechanism, the fund will achieve significant financial leverage through its support of bright early-career researchers enhancing their ability to obtain career-defining long-term research funding. The potential to follow these advanced individuals and maintain relations with them as they grow in their career is invaluable. With a 3-year commitment, we look forward to funding three Graeme McDaniel Research Scholars.
"Complex congenital heart disease (CHD) patients invariably require complicated surgical repairs. Despite the best possible surgical repair, some of the patients develop heart failure. My research is focused on applying cutting edge genomic tools to understand why the heart muscle fails in these patients. The CHD heart muscle faces abnormally high amounts of stress and works tirelessly, and our recent results show that the CHD heart muscle ages faster than expected. Now that we have an insight into why these CHD hearts fail, we can start working on making the heart muscle stronger [by using precision medicine]." Dr. Turaga
You can read more about Dr. Turaga’s work in his Nature paper and in this interview.
Diwakar Turaga, MD, PhD Assistant Professor of Pediatrics, Section of Critical Care Medicine, Baylor College of Medicine